Nontyphoidal Salmonella infections in CT — Decreasing antibiotic susceptibility and increasing antibiotic use
The Centers for Disease Control and Prevention (CDC) has designated drug-resistant nontyphoidal Salmonella as a serious public health threat in their Antibiotic Resistance Threats in the United States, 2019 report (1) based on data from the National Antimicrobial Resistance Monitoring System for Enteric Bacteria (NARMS). NARMS was implemented in 1996 to monitor changes in antimicrobial susceptibility among enteric pathogens, including nontyphoidal Salmonella, by testing isolates from across the country (2). These national data highlighted changes in susceptibility to commonly prescribed antibiotics including ciprofloxacin. Nationally, the proportion of nontyphoidal Salmonella isolates with decreased susceptibility to ciprofloxacin increased from 2% to 8% between 2009-2017(1). Since 1995, Connecticut has participated in the Foodborne Diseases Active Surveillance Network (FoodNet), a collaborative effort between CDC, 10 Emerging Infections Program (EIP) sites, the US Department of Agriculture (USDA), and the Food and Drug Administration (FDA), to monitor the burden of enteric diseases, including salmonellosis (4). This has provided an opportunity to better understand severity of illness, potential exposures before infection, and history of antibiotic use. This is important in the context of antibiotic resistance. Pathogens with decreased susceptibility may lead to more severe disease, including hospitalization; overuse of antibiotic treatment can contribute to antibiotic resistance; and exposures known to be associated with decreased susceptibility or resistance can help narrow down treatment options if antibiotics are recommended (1).Treatment of nontyphoidal Salmonella infection with antibiotics is generally not recommended but may be recommended for case-patients who experience severe illness, are at least 65 years of age, or are immunocompromised (5).
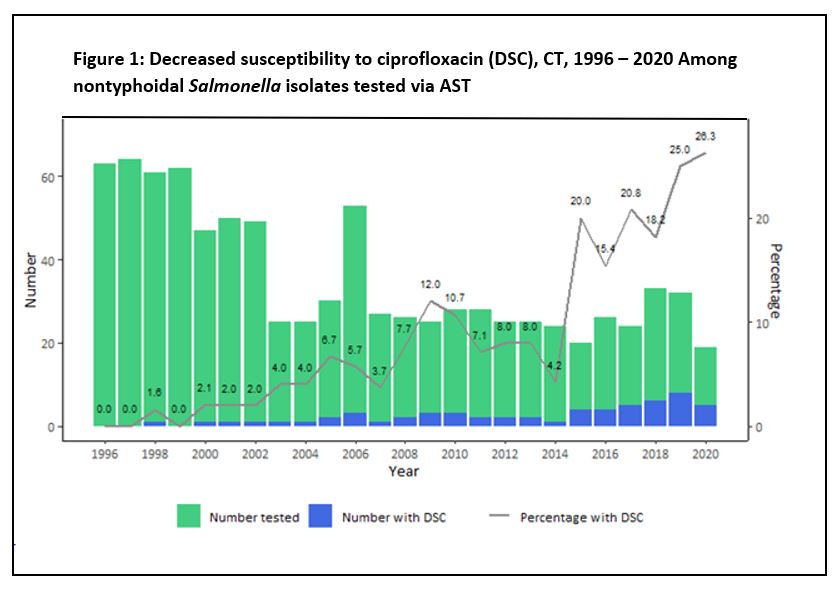
Using both Connecticut NARMS and FoodNet case interview data, we evaluated trends in ciprofloxacin susceptibility among nontyphoidal Salmonella isolates and antibiotic use among salmonellosis case-patients. We also assessed associations between ciprofloxacin susceptibility and international travel and illness severity using hospitalization as a marker. NARMS susceptibility data on Connecticut nontyphoidal Salmonella surveillance isolates collected during 1996-2020 were analyzed. Decreased susceptibility to ciprofloxacin (DSC) was defined according to the Clinical and Laboratory Standards Institute (CLSI). Isolates with minimum inhibitory concentration (MIC) values in the intermediate (MIC = 0.12–0.5 μg/ml) or resistant (MIC ≥1 μg/ml) range were considered to have decreased susceptibility (3). FoodNet data on hospital admission and international travel among nontyphoidal Salmonella cases were available for 2010-2021 and on antibiotic usage for 2018-2021. Chi-square for trend tests were used to analyze yearly trends in the proportion of isolates with DSC and in antibiotic use among cases. The association between DSC and hospitalization status and international travel were assessed via the chi-square test.
Between 1996-2020, the proportion of isolates with DSC increased significantly from zero to 26.3% (chi square for trend = 58.97, p < 0.001) (Figure 1). Infections caused by Salmonella with DSC were found to be significantly associated with international travel, with 28.6% (10/35) of case patients with DSC infections having traveled within the seven days prior to illness onset, compared with 13.7% (25/183) of those with ciprofloxacin susceptible infections (chi square = 4.85, p<0.05). Among case-patients reporting international travel, most had traveled to Central America, South America or the Caribbean, although there was not a significant association between DSC and travel to any particular region. No significant association was found between infection with Salmonella with DSC and hospitalization status, with 38.2% (13/34) of those with DSC infection being hospitalized compared with 34.4% (64/186) of those with ciprofloxacin susceptible infection (p-value=0.67).
Connecticut FoodNet data from 2018-2021 were used to identify the proportion of salmonellosis case-patients that reported using antibiotics to treat their infection. Across all four years, the proportion treated with antibiotics was 50.4% (904/1795), increasing from 47.2% (236/500) in 2018 to 56.0% (241/430) in 2021 (chi square for trend = 5.87, p<0.05). Among those treated with antibiotics, 377 (41.7%) were hospitalized, 189 (20.9%) were 65 years or older, and 465 (51.4%) were either hospitalized, 65 years or older, or both. Ciprofloxacin was the most commonly reported antibiotic with 15.8% (n=283) of all case-patients and 31.3% of case-patients on antibiotics treated with it.
Editorial
Connecticut has seen a rise in levels of DSC among nontyphoidal Salmonella infections, increasing beyond the 2017 national level of 8% (2). In 2017, over 20% of nontyphoidal Salmonella infections in Connecticut had DSC; this percentage increased to over 25% in 2020. This level of decreased susceptibility, and the trajectory of it, is concerning, especially when coupled with the fact that the most commonly prescribed antibiotic reported in Connecticut for nontyphoidal Salmonella infection from 2018-2021 was ciprofloxacin. However, given that fluoroquinolones are among the recommended first line therapies for empiric treatment of Salmonella infection, this is not surprising, and is in agreement with recommendations.
While we did not see increased hospitalization rates among DSC infections in Connecticut, further analysis is needed to explore other indicators of severe illness. Increasing rates of antibiotic treatment may be in response to increasing disease severity that is not reflected in hospitalization rates, however that is beyond the scope of this analysis. Analysis of Connecticut data shows an association between DSC and international travel. According to the 2018-2019 FoodNet Population Survey, international travel in the past 30 days was more commonly reported among Connecticut residents (5.0%) compared to the overall percentage among residents of all FoodNet sites (3.7%) (6). This suggests that international travel may play a role in the higher proportion of DSC in CT than in the US overall.
Healthcare providers should evaluate the need for antibiotics when caring for patients with nontyphoidal Salmonella infection, as treatment may not be recommended for all patients. This is of utmost importance as prudent use of antibiotics can help mitigate the serious public health threat of antibiotic resistance. Further recommendations can be found in the 2017 Infectious Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Management of Infectious Diarrhea (7).
Reported by
A Edmundson, MPH, P Gacek, MPH, Q Phan, MPH, Connecticut Department of Public Health
Acknowledgements
C Nishimura; Connecticut State Public Health Lab; T Rissman; Connecticut Department of Public Health Epidemiology and Emerging Infections Program; FoodCORE
References
- CDC. Antibiotic Resistance Threats in the United States, 2019. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf. Accessed June 2, 2022.
- CDC. National Antimicrobial Resistance Monitoring System for Enteric Bacteria (NARMS). https://www.cdc.gov/narms/index.html. Accessed June 2, 2022.
- FDA. 2018 NARMS Update: Integrated Report Summary. 2018 NARMS Update: Integrated Report Summary | FDA. Accessed August 31, 2022.
- CDC. Foodborne Diseases Active Surveillance Network (FoodNet). https://www.cdc.gov/foodnet/index.html. Accessed June 2, 2022. CDC.
- Salmonella: Information for Healthcare Professionals and Laboratories. https://www.cdc.gov/salmonella/general/technical.html. Accessed June 2, 2022.
- CDC. FoodNet Fast’s Population Survey Tool. https://wwwn.cdc.gov/Foodnetfast/PopSurvey. Accessed June 6, 2022.
- Shane AL, Mody RK, Crump JA et al., 2017 Infectious Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Management of Infectious Diarrhea, Clinical Infectious Diseases, Volume 65, Issue 12, 15 December 2017, Pages e45–e80, https://doi.org/10.1093/cid/cix669
This page last updated 03/28/2023.

