Think about YOURSELF.
Think about SOMEONE YOU LOVE.
- Connecticut has the 2nd highest incidence (number of new cases) of breast cancer in the United States.
- In 2024, it is estimated that there will be 3,790 new cases of female breast cancer in Connecticut and 420 females will die from breast cancer.
- From 2020 to 2021, the incidence of breast and cervical cancer increased by 15% and 12% in Connecticut.
- From 2020 to 2021, breast cancer cases among Connecticut residents aged 20-39 increased by 28%.
- Hispanic women are diagnosed with cervical cancer more often than all other races and ethnicities in Connecticut.
- Non-Hispanic Black women in Connecticut are more likely to die from breast and cervical cancer when compared to all other races and ethnicities.
The Connecticut Breast and Cervical Cancer Early Detection Program (CBCCEDP) serves about 5,000 Connecticut residents every year. We have helped around 80,280 people visit doctors, get mammograms, pap tests, HPV tests, and more.
The Connecticut Breast and Cervical Cancer Early Detection Program
The Connecticut Breast and Cervical Cancer Early Detection Program (CBCCEDP) is a comprehensive screening program available throughout Connecticut for medically underserved women. The primary objective of the program is to significantly increase the number of women who receive breast and cervical cancer screening, diagnostic and treatment referral services. All services are offered free of charge through the Connecticut Department of Public Health’s contracted health care providers located statewide.
The CBCCEDP Screening and Diagnostic Services is for women 21-64 years and include:
| Office Visits | Colposcopies and Colposcopy-Directed Biopsies |
| Screening and Diagnostic Mammograms | Loop Electrode Excision Procedure (LEEP) |
| Breast Biopsies | Surgical Consultations |
| Breast Ultrasounds | Clinical Breast Exams |
| Fine Needle Aspirations | HPV Screening (human papilloma virus) |
| Pap Tests | Cardiovascular Screening |
Who Can Enroll?
You are eligible for program services if:
- You are 21-64 years old
- 21-64: Clinical Breast Exam & Pap Test
- 40-64: Mammogram
- You are 35-39 with symptoms or specific risk factors for breast cancer
- Examples: genetic mutations, dense breasts, personal & family history of breast or cervical cancer
- You are at or below 250% of the Federal Poverty Level – See chart below , and
- You have no health insurance, or
- You have health insurance that excludes routine Pap Tests and/or Mammograms
- You have an insurance deductible of $1,000 or more, or
- You have no Medicare Part B
*Women 65+ who are not enrolled in Medicare Part B may be eligible to receive CBCCEDP services.
FEDERAL & STATE INCOME ELIGIBILITY GUIDELINES
(Based on 250% of the 2024 Federal Poverty Guidelines)
*Household gross income must be less than or equal to the following:
|
Family Size |
Annual Income |
Monthly Income |
Biweekly |
Weekly Income |
|
1-person family |
$37,650 |
$3,138 |
$1,448 |
$724 |
|
2-person family |
$51,100 |
$4,258 |
$1,965 |
$983 |
|
3-person family |
$64,550 |
$5,379 |
$2,483 |
$1,241 |
|
4-person family |
$78,000 |
$6,500 |
$3,000 |
$1,500 |
|
5-person family |
$91,450 |
$7,620 |
$3,517 |
$1,758 |
|
6-person family |
$104,900 |
$8,741 |
$4,034 |
$2,017 |
|
7-person family |
$118,350 |
$9,862 |
$4,551 |
$2,275 |
|
8-person family |
$131,800 |
$10,983 |
$5,069 |
$2,534 |
|
9-person family |
$145,250 |
$12,104 |
$5,586 |
$2,793 |
|
10-person family |
$158,700 |
$13,225 |
$6,103 |
$3,051 |
|
For each additional family member add: |
$13,450 |
$1,121 |
$517 |
$259
|
Contact Us or the Program Center in Your Local Area
Contact Us by Email:
To learn more, send your first name with your phone number or email address to the Connecticut Early Detection and Prevention Program (CEDPP).
Call Any of the Following Locations:
The Connecticut Department of Public Health, 860-509-7804 or
Contact your local health care provider program listed below.
|
TOWN |
LOCATION |
PHONE |
|
Bridgeport |
Bridgeport Hospital |
(203) 384-3392 |
|
Danbury/Norwalk/ New Milford |
NUVANCE/WCHN |
(203) 739-4770 |
|
Putnam |
Hartford HealthCare |
(860) 823-6534 |
|
Hartford |
Hartford HealthCare |
(860) 972-3078 |
|
Hartford |
St Francis Hospital |
(860) 714-7151 |
|
Stafford |
Johnson & Memorial |
(860) 714-9071 |
|
Waterbury, Vernon, South Windsor |
Prospect/ECHN/Waterbury Hospital/Rockville Hospital/Manchester Hospital |
(860) 872-5368 (866)660-8837 |
|
Meriden |
MidState Medical Center |
(860) 972-1900 |
|
New Haven |
Yale New Haven Hospital |
(203) 688-2219 |
|
New London |
Lawrence & Memorial Hospital |
(860) 442-0711 x2197 |
|
Norwich |
Backus Hospital |
(860) 823-6539 |
|
Torrington |
Charlotte Hungerford Hospital |
(860) 496-6513 |
|
Uncas Health District |
Uncas Health District |
(860)639-5138 |
|
Waterbury |
St. Mary's Hospital |
(203) 709-3795 |
|
Waterbury |
Waterbury Hospital |
(860) 872-5368 |
|
Willimantic |
Windham Hospital |
(860) 823-6354 |
This list does not include of all clinics that provide these services. There many be a clinic closer to you.
Call the location closest to you and they will direct you to the closest clinic.
| For more information, please see the CEDPP brochure (English, Spanish, Portuguese, LGBTQ+). |
Breast & Cervical Cancer Risk Factors
Genetic Risk Factors
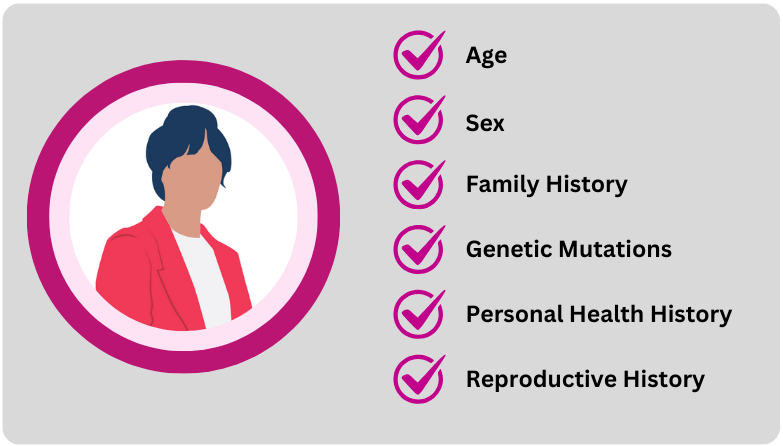
Age: As you get older, your risk for breast cancer increases. Most breast cancers are diagnosed after age 50. About two out of three invasive breast cancers are found in people 55 or older.
Sex: Women or people assigned female at birth are are 100x more likely to be diagnosed with breast cancer than men or people assigned male at birth.
Family History: Having a close relatives, especially sisters, mothers, or daughters, who have been diagnosed with breast or cervical cancer may increase one’s risk for breast and cervical cancer. Your risk increases if your relative was diagnosed before the age of 50.
Genetic Mutations: Certain DNA changes that increase the risk of breast cancer, such as BRCA1 and BRCA2, can be passed from parents to children.
Personal Health History: People who have had breast cancer are 3-to-4 times more likely to get breast cancer a second time. People with dense breasts are also more likely to get breast cancer.
Reproductive History: Starting menstrual periods before age 12 and starting menopause after age 55 expose people to hormones longer, raising their risk of getting breast cancer.
Genetic risk factors cannot be changed because they are built into you DNA. They are passed down from your parents. Although they cannot be changed, their risk level can be reduced through changes in your lifestyle and environment.
Environmental and Lifestyle Risk Factors
That YOU can change!

Not being physically active: People who are not physically active have a higher risk of getting breast cancer. Moving your body or exercising for even 20 minutes a day can help lower this risk factor.
Poor Diet: A diet high in saturated fat and low in fruits and vegetables can increase your risk for breast and cervical cancer. Eating 3.5 to 5 cups of fruits and vegetables a day can help lower this risk factor.
Being overweight or having obesity after menopause: Older people who are overweight or have obesity have a higher risk of getting breast cancer than those at a healthy weight.
Taking hormones: Some forms of hormone replacement therapy (those that include both estrogen and progesterone) taken during menopause can raise risk for breast cancer when taken for more than 5 years. Certain oral contraceptives (birth control pills) also have been found to raise breast and cervical cancer risk. An intrauterine device (IUD) is a form of birth control that may lower risk of cervical cancer.
Human papillomavirus (HPV) infection: HPV is a group of more than 150 related viruses that can eventually cause certain cancers, such as cervical cancer. HPV can spread from one person to another during skin-to-skin contact. HPV vaccines are available to help prevent infection by certain types of HPV and some of the cancers linked to those types.
Reproductive history: Having the first pregnancy after age 30, not breastfeeding, and never having a full-term pregnancy can raise breast cancer risk. While having 3 or more full-term pregnancies, having your first full-term pregnancy before the age of 20, becoming sexually active at a young age and having many sexual partners can increase the risk of cervical cancer.
Drinking alcohol: Studies show that a person's risk for breast cancer increases with the more alcohol they drink.
Smoking: Smoking is linked to a higher risk of breast and cervical cancer in younger, pre-menopausal women.

